Quality laboratory diagnostics is critical for improving patient outcomes. Yet issues with reproducibility and high-profile cases of misdiagnosis have raised questions about the validity of today’s diagnostic testing. Without guaranteed quality, patients can experience life-limiting outcomes and researcher’s experiments often cannot be reproduced.
So what exactly is quality in diagnostics labs, and how can you ensure your results are the best possible quality?
What is laboratory quality – and how does it impact diagnostics?
In diagnostics, ‘laboratory quality’ refers to the accuracy and precision of the reported diagnostics test results.
Ideally, lab results should be correct 100% of the time. But ensuring this level of quality is near-impossible, and even if 99% of results are accurate it can be catastrophic – something we’ve learned from inaccurate COVID-19 tests.
Any number of analytical, pre-analytical and post-analytical errors – from human mistakes, equipment errors and sample preparation failure – can mean that tests aren’t providing the correct results. When tests are regularly incorrect, laboratory quality is impacted.
Tests can be wrong for a number of reasons: A scientist manually processing tests might miss out on pipetting the sample into a well; cross-contamination can impact the results; or measurements made by researchers can be inaccurate.
In many cases, it’s impossible to even know how many tests are failing, or what the quality of a lab’s output is until the results impact something. Because human error is such a big factor in the quality of results, the number of inaccurate tests that are uncovered could only show a small percentage of the total tests.
Why is quality valued as an important aspect in diagnostics labs?
Accurate test results play an important role in spotting health problems and informing medical intervention. It’s estimated that 70-80% of all healthcare decisions affecting diagnosis or involve a pathology investigation. And, as diagnostics methods become more advanced and healthcare demand grows, the need for tests is increasing.
Early diagnosis is also critical to providing better outcomes for patients. Quality testing is a big part of ensuring diagnostic testing is timely, since a high number of failed tests can mean constant re-testing and valuable time being wasted in failure analysis.
Reproducibility is another element of diagnostic testing that is impacted by poor-quality lab results. For science to advance, researchers must be able to repeat and corroborate each other’s experiments. Yet, in a Nature poll of 1,500 scientists, 70% reported failing to reproduce another scientist’s experiments, and more than half have failed to recreate their own.
Much of this issue can be attributed to poor-quality lab results. Without quality results being ensured in experiments, time and resources are wasted, and false leads are pursued.
Since fast and accurate diagnosis can mean the difference between life and death, and the advancement of the diagnostics field as a whole, labs must rapidly evolve to improve the accuracy and reliability of test results. So let’s take a look at some of the ways to ensure quality in laboratory diagnostics.
Approaches for ensuring laboratory quality
Quality is a critical part of any diagnostics lab’s ability to treat patients effectively, and ensure its reputation in the field.
There are a number of approaches that can be taken to increase the quality of a diagnostic laboratory’s output, including:
- Internal quality control (IQC): IQC is an internal check that a laboratory will produce the same result or outcome if the test or procedure is done on different occasions
- External quality control (EQC): EQA schemes are when an external peer group of laboratories compare the labs testing to a source outside of the laboratory to ensure that their results are quality
- Staff training: Since much of quality in diagnostic testing comes down to human error, staff must be trained to a high standard to ensure precision of work
- Equipment maintenance: To avoid any potential downtime or machine error, equipment and instruments should have regular preventative maintenance carried out
- Reducing manual processes: Errors normally happen in the lab because humans aren’t built to conduct manual tasks, like pipetting, over and over again. By automating these kinds of tasks, diagnostic testing quality can be significantly improved
When it comes to improving quality in diagnostics, eliminating manual processes is one of the most effective methods to provide better patient outcomes and more reproducible results. And automation is the best way to reduce the human error that manual testing causes.
How automation makes diagnostic labs’ results more accurate, precise and timely
Human error is very difficult to manage, after all, ‘to err is to human’. It’s also very common in diagnostics labs where highly repetitive, exhausting tasks make up the bulk of the work in processing tests.
When automation is used for highly repetitive processes, such as preparing samples for analysis, there are many benefits:
- With human error eliminated, lab results are more accurate and precise
- Re-testing isn’t necessary and diagnosis can be delivered faster
- Labs are far more efficient, saving time, money and resources while improving patient outcomes
- Experiments are much more precise and therefore reproducible
- Hugely reduced chances of cross-contamination
- Safety of staff can be ensured because they are spending less time handling potentially infectious samples
- Better work life for staff, with fewer monotonous jobs, less exhaustion and walkaway time ensured so they can focus on the work that really matters
Yet, despite the benefits automation brings to laboratory quality, the field has been surprisingly slow to automate. Unfortunately, automation has traditionally been too complex, inflexible and expensive for use in the lab space.
Lab automation shouldn’t be so difficult, and it doesn’t need to be intimidating. It’s a powerful way to empower labs to create better results and supercharge patient care and scientific innovation.
In the last section, we look at how to pick an automation solution that’s right for you.
Boost Genomics Testing Capacity in Public Healthcare
Discover how integrated automation can triple throughput, reduce costs, and streamline workflows for genomics labs.
Finding an automation solution that’s right for your lab
There are three key factors you should consider when looking for a lab automation solution that’s going to effectively increase quality in your diagnostics lab:
Flexibility: Your automation requirements may change, so you need to find a solution and vendor that can be flexible for your changing needs
Complexity: Traditional automation solutions often require an expert with decades of experience to deploy and manage. Finding a solution that is simple enough for your existing staff to use and can be deployed in just a few weeks or months is critical. Managed services are a good option for automation beginners to consider
Cost: Traditional automation solutions can often cost up to the millions to be deployed. Shop around for more affordable solutions – newcomers to the space can often provide more innovative solutions for a lower price tag.
Meet LINQ – the complete workflow automation platform
Automata’s LINQ platform houses and connects your instruments on a space-saving, robot-enabled lab bench, while allowing you to design, schedule and manage workflows remotely via cloud-based software. Underpinned by your lifetime support team of scientists, engineers and automation experts, LINQ is the last automation solution you’ll ever buy.
In diagnostics, ‘quality’ refers to the accuracy and precision of the reported diagnostics test results.
Addressing QC issues in a diagnostic laboratory is critical to the identification of potential errors with patient results, including reagent matrix effects as well as calibration misalignment of testing function. Maintaining accurate and frequent checks of laboratory sample testing through quality control is vital to ensuring that patient testing is done right and that it produces accurate results. When quality control works effectively, it is able to find and correct flaws in the analytical processes of a lab before potentially incorrect patient results are released
Quality control involves inspecting specimens, reviewing transcriptional measures, using the most reliable tests and verifying final results. While benchtop automation improves the reliability and efficiency of processes in the lab, full automation across workflows end to end is the best way to remove the risk of contamination, to improve the reproducibility, and tracibility of experimentations.
Quality control in diagnostic laboratories is important for many reasons, from certification and accreditation to the accuracy and reproducibility of results. When quality control works effectively, it is able to find and correct flaws in the analytical processes of a lab before potentially incorrect patient results are released.
Nick Lench, Genomics Expert and Co-Founder of Congenica, discusses the challenges holding…
Read more Enabling clinicians and patients to make data-driven decisions with genomics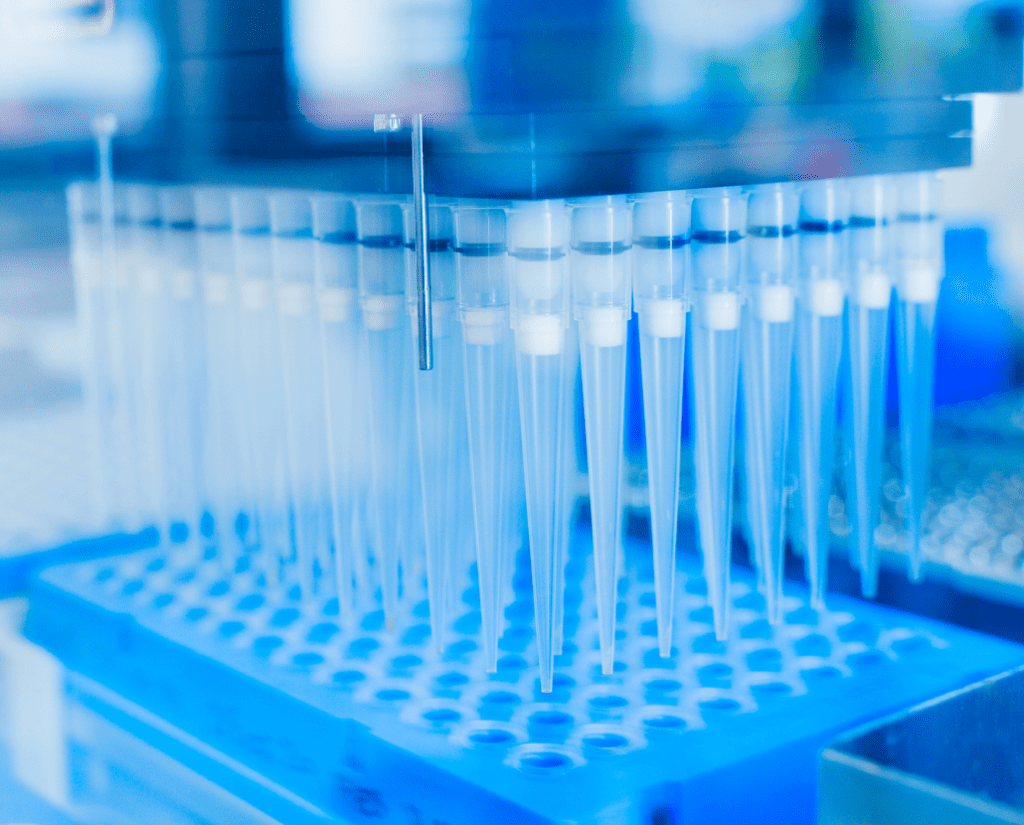
Lab automation technologies reduce the pressure on repetitive tasks, increase productivity and…
Read more The benefits of lab automation for diagnostic testing